Jeonju Community-based Integrated Care Program
The concept of community-based integrated care is gradually replacing facility-based care. Community-based integrated care can be defined as local community-based social services that provide homecare and health, and medical services with the aim of enabling community residents to live in their own homes. While it maximizes the utilization of community resources to support older people, it can also act as a safety net in emergencies, those created by poverty and, for instance, COVID-19. Leading welfare states such as the U.K., Japan, and Sweden are already transitioning to community-based services. The U.K. enacted a Community Care Law in the 1990s and has actively implemented community care. Japan adopted a municipal integrated care system in 2013, establishing community-based integrated care. Sweden passed a Social Service Law (Socialtjänstlagen) in 2001, empowering regional governments to take more responsibility for long-term care.
South Korea, on the brink of a super-aged society, recently recognized the need for community-based integrated care. In 2019, the Korean government selected five municipalities (Gwangju Seo District, Bucheon, Cheonan, Jeonju, and Kimhae) to introduce community-based integrated care programs for older people. For four years, since 2019, Jeonju has conducted the Jeonju Community-based Integrated Care Program, constructing integrated care systems within the region. For effective implementation, Jeonju has established private-sector support groups and six administrative committees. Those who participate in the private-sector support groups include medical facilities such as hospitals, traditional Korean medical clinics known as Haneuiwon, and pharmacies. Currently, the Ministry of Health and Welfare is developing a nationwide integrated care model, using Jeonju's integrated care program as the benchmark. Other municipalities, such as Yeoju and Gwangju, are trying to introduce several elements of Jeonju's integrated care.
The Jeonju community-based integrated care program introduced a number of features from the Japanese model, which focuses on preventive medical care and aims for 'ageing in place.' The Jeonju program has developed a medical safety net in order to improve the health of older people while reducing medical expenses. In 2022, Jeonju implemented 29 programs for older people; they include medical care, dementia and pharmaceutical services, nutritional information, housing services, support groups, and physical activities.
A key program among all 29 programs is the Health-medical SafetyNet program, which involves the cooperation of the Doctors' Association, the Social Healthcare Association, Jeonju Presbyterian Medical Center, and public community health centers. The program puts health improvement and preventive care at its core. For severely ill patients, it offers home care and intensive care.

One of the notable elements of Jeonju community-based integrated care is that it provides services through a classification system that measures older persons' needs. For example, an older person might require intensive care or, on the other hand, be ready to leave the hospital. Classification is based on tests and questionnaires, which include the FRAIL scale and tests for depression and dementia. The results are analyzed using statistical methods, with standardizing and weighted means. In 2021 the number of older people participating in the program was 1,867, and the goal for 2022 was 2,660.
Another distinctive element of the Jeonju program is the Supporters Program. Jeonju Community-based Integrated Care Supporters are selected participants in senior employment programs. They are all retired workers with high expertise. The Supporters provide various services for the program, including direct care in homes, befriending, campaigning publicly in support of the program, and many more. The goal is to build a healthy local community through older people themselves. In 2022, 274 older people participated as Supporters. Jeonju has reached a Memorandum of Understanding with the Ministry of Health and Welfare to expand the Supporters model nationwide.

It is four years since Jeonju first introduced a community-based integrated care program. Has it been effective? Evaluation in 2020 suggested 72.68 percent of participants responded that they were happier than before the program began. But to find out whether the program has increased older people's well-being in physical and economic aspects, we needed concrete evidence of both improvements in their health and reduced medical costs.
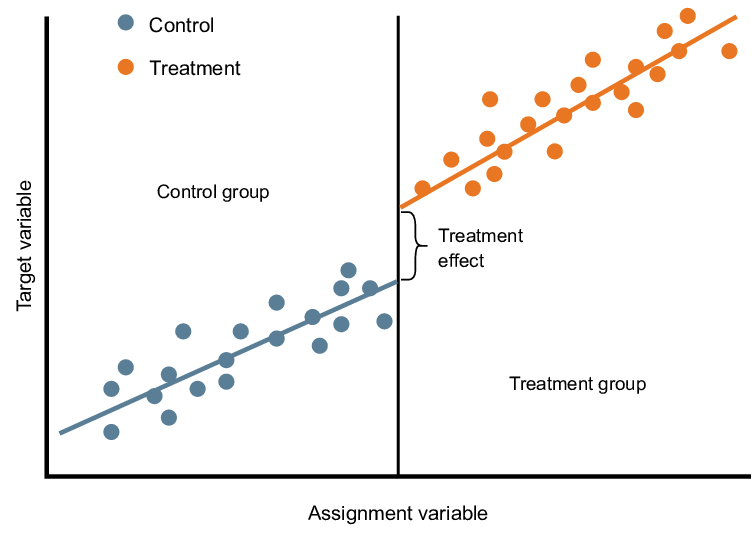
In 2020, Seoul National University evaluated Jeonju's program using Regression Discontinuity Design (RDD) and Bayesian Network Analysis (BNA). RDD measures a program's impact by dividing a similar population into participants and non-participants. RDD measured if there were any differences in specific variables between the groups after the program began. (See the picture below) The RDD analysis showed that the cost of individual health insurance paid by NHIS (National Health Insurance Service) was reduced by approximately $2000. The hospital admission fee per participant was also reduced by about $300. The BNA tests whether variables have a connected relationship and dependency. The BNA result showed that the program affects variables such as health management and lifestyle, which positively impact physical health. Thus, we could say that Jeonju's program had an actual positive impact.
Although Jeonju has successfully introduced community-based integrated care, some argue it needs improvement in several areas. First, the program has experienced increased participation and expanded its services for four years, but the pandemic increased the workload and put pressure on the workforce. Some suggest that additional coordination between human resources and services is required. Second, because the South Korean mainstream medical system is facility-based, it tends to put older people into facilities. The parallel implementation of community-based integrated care programs and facility-based institutions might lead to situations where older people with an immense need for integrated care go into the facility while others with relatively better conditions get selected for the program. This needs to be addressed during the process of expanding the community-based integrated model nationwide.
According to the report of the Korea Institute of Health and Social Affairs, 69.4 percent of older people said that homecare was the most essential requirement for 'ageing in place.’ Community-based integrated care is trying to meet this demand by concentrating on preventive care to reduce the need for facility-based care, providing a total package of medical and health services. Now the Ministry of Health and Welfare is expanding the model nationwide, on a bigger scale and with more complexity. As Korea sets out on the path to community-based integrated care, Jeonju's model is likely to find itself increasingly used as the benchmark for the rest of the country.